The Architecture for Pandemic Prevention, Preparedness, & Response (PPPR): Views from Civil Society Leaders on the UN High Level Meetings [GUEST ESSAY]
Newsletter Edition #42 [Treaty Talks - Featured in GHF]
Hi,
Health continues to dominate political agendas globally, even as urgency in the response to COVID-19, seems to be ebbing away. Last week WHO indicated how few countries are sharing information on reporting deaths from the disease and on sequencing, for example.
So even as countries meet in New York next week for a packed calendar of the UN High Level Meetings, and as negotiations on the Pandemic Accord gather steam in Geneva, that the painful lessons from COVID-19 will be effectively incorporated into future actions is far from clear.
In today’s edition, practitioners and experts from civil society organizations urge countries to improve on community engagement, financing and to learn from what we already know while designing future roadmaps for Pandemic Prevention, Preparedness, & Response. Read on.
If you find our work valuable, become a paying subscriber. Tracking global health policy-making in Geneva is tough and expensive. Help us in raising important questions, and in keeping an ear to the ground. Readers paying for our work helps us meet our costs.
Until later.
Best,
Priti
Feel free to write to us: patnaik.reporting@gmail.com or genevahealthfiles@protonmail.com; Follow us on Twitter: @filesgeneva
I. GUEST ESSAY
Featured in Geneva Health Files: Sponsored Series
The Architecture for Pandemic Prevention, Preparedness, & Response (PPPR): Views from Civil Society Leaders on the UN High Level Meetings
Coalition of Advocates for Global Health and Pandemic Preparedness
Mitchell Warren, AVAC; Robin Gorna, Frontline AIDS; Cindy Kelemi, BONELA; Chris Collins, Friends of the Global Fight; Florence Riako Anam, Global Network of People Living with HIV; Amira Herdoiza, Kimirina; Rosemary Mburu, WACI Health; Mike Podmore, STOPAIDS; Katy Kydd Wright, Global Fund Advocates Network
For months, we have watched as Member States have tried to negotiate a UN Political Declaration on Pandemic Prevention, Preparedness, and Response (PPPR) ahead of the UN High Level Meeting in September.
With groups of Member States at odds on equity issues, these negotiations have gone severely off track.
This is the time to deliver a Political Declaration that is ambitious, timely, and in pursuit of a level of equity that has yet to be achieved in global health. As Directors of civil society and community organizations working globally on health, the HIV response, and pandemic preparedness, we see and experience first-hand the risk of failing to deliver, particularly for marginalized, criminalized, and under-resourced communities.
We are founding members of the Coalition of Advocates for Global Health and Pandemic Preparedness and have engaged with the multiple initiatives that have arisen in the wake of the COVID-19 pandemic, including ACT-A, the Pandemic Fund launch, the Pandemic Accord, the UN High Level Meeting on PPPR, and the development of a medical countermeasures platform.
Our aim is to ensure increased and meaningful involvement of civil society and communities in the development and decision-making of these initiatives and to advocate for an integrated and holistic approach to pandemic preparedness that emphasizes equity, diversity, inclusion, global solidarity, and synergies of multiple existing global health programs. With the final draft of the PPPR Political Declaration now circulated to Member States, we have four key asks of Member States in adopting and implementing these commitments.

First, the Declaration includes an important recommitment to ending the epidemics of HIV, tuberculosis, and malaria while drawing from their wealth of experience in designing future pandemic responses. Much of the pandemic preparedness infrastructure that countries recognize is needed – such as surveillance structures, laboratories, and testing centers – has been supported as part of the responses to these three epidemics. These platforms must be built upon and expanded.
In addition to dedicated investments in pandemic preparedness, ongoing epidemic responses should be leveraged and expanded, saving time and money and incorporating program values of community inclusion, reaching the most marginalized, transparency and inclusive decision-making, and accountability for impact. Civil society and communities play a critical role in prevention, preparedness and response. While it has taken decades to secure this inclusion in AIDS, TB, and malaria responses, many of these programs now offer a pathway to broad stakeholder engagement, including recognition of civil society and communities as decision-makers with formal representation in governance structures. This must also be considered a baseline level of engagement in global and country-level PPPR structures going forward.
Second, the current Declaration fails in its commitments to equity in responses to future pandemics. Equity issues have been a source of major areas of disagreement in the negotiations leading up to the Declaration’s adoption. It is imperative that we build a system which prioritizes the fair, timely, and sustainable allocation of medical countermeasures in the event of a pandemic threat.
In the peak of COVID-19, countries rushed to secure advance purchase agreements of promising candidates for effective vaccines, putting whichever countries could pump the most cash, to the front of the queue to claim what supply would be available. This resulted in many countries with less liquid cash flows to wait many months and even years to get their first formal shipments outside of donations.
We call on Member States to establish an ambitious and equity-centered approach to responding to pandemics of the future, and the present. We look to the INB process of the Pandemic Accord to find consensus on these issues.
Thirdly, we call on Member States to invest in community-led structures as an integral piece of preparedness. This goes beyond the current references to community-based primary care, which is distinct from and often wrongly conflated with health responses which are truly led and developed within and by communities and civil society.
As demonstrated during COVID-19, community-led responses are essential in preventing, detecting, and responding to pandemics, particularly for marginalized populations. A successful response starts and ends with communities, from identifying a possible outbreak to delivering vaccines in underserved populations. However, for these community systems to remain resilient in the face of a pandemic threat, there must be ongoing investment in strengthening their financing, their infrastructure, and their meaningful engagement. It is vital that the Declaration supports this, and includes commitments to supporting efforts that are truly community-led.
Lastly, the Declaration recognises the need for financial and investment commitments (including through enhanced official development assistance and adequate surge financing for future responses, and other means of innovative financing), but Member States must commit to additive and sustainable financing rather than siphoning off current global health investments. In order to move beyond the cycle of panic and neglect, we must get away from forcing global health priorities to compete against each other for funding. Countries must invest adequately in global health now. The problems that collectively face us cannot be solved with a one-time contribution.
The Declaration should act as a catalyst to recommit Member States to mobilizing financing for PPPR across different vehicles, including the Pandemic Fund, Global Fund to Fight AIDS, TB, and Malaria, Unitaid, and WHO Contingency Fund, and through innovative methods such as expanding use of multilateral development banks, debt relief for health agreements, and catalytic finance platforms.
We call on Member States to commit to these actions in order to achieve the goals laid out in the Declaration. Building on what we have, centering equity, diversity, and meaningful inclusion in our global and country-level PPPR architecture, strengthening community engagement, and sustainably financing global health are crucial to the world’s success. With a more equitable, inclusive, integrated, and well funded system we can prevent outbreaks, prepare for inevitable threats, respond to pandemics, and work to end the epidemics of today.
Get in touch with the authors via : Eolann Mac Fadden <emacfadden@frontlineaids.org>; Samantha Rick <samantha@avac.org>
As announced earlier, this is a part of the Featured in Geneva Health Files Sponsored Series that enables stakeholders to communicate with our painstakingly-built audience of more than 5,000 readers across 130 countries comprising decision-makers, diplomats, academia, experts, activists and the private sector. It also helps us diversify our revenues. We address sponsored content on a case-by-case basis, with care, caution, responsibility and discretion, in line with our editorial policy. Write to us if you wish to engage with our readership.
II. PODCAST CORNER
Navigating Digital Health Waves
Join Global Health Matters in this podcast episode to develop a broader understanding of how health is being shaped through digital technologies.
Increasingly, digital technologies are transforming the delivery of health services and the functioning of health systems. Many of these technologies have also presented new ways of doing research and informed rapid decision-making. This episode discusses how UNICEF worked with Jamaica to rapidly deploy an electronic registry solution for the COVID-19 vaccine. In addition, we also learn about how the government of Philippines created an opportunity for research by allowing open access to data based on COVID-19 tests.
Host Garry Aslanyan speaks with the following guests:
Karin Källander: Senior Health Adviser and Chief of the Digital Health & Information Systems Unit, UNICEF
Alvin Marcelo: Executive Director of Asia eHealth Information Network and Chief Medical Information Officer of St. Luke's Medical Center in the Philippines
Garry Aslanyan is the host and executive producer of the Global Health Matters podcast. You can contact him at: aslanyang@who.int
[This is a sponsored advertisement: Get in touch with us if you want to promote books, webinars, job postings. Write to patnaik.reporting@gmail.com.]
III. WHAT WE ARE READING
G20 New Delhi Leaders’ Declaration
Unprecedented focus on global public health at UN General Assembly: WHO
Former UK PM Gordon Brown calls for new era of international cooperation, multilateralism: WTO
WHO Announces Air Pollution Summit in Accra to Tackle ‘Public Health Emergency’: Health Policy Watch
A Blueprint for Inclusive Health Architecture: Insights from India's G20: Global Health Now
IV. WE ARE KEEPING AN EYE ON:
WHO: 15 September
INB Informal meeting on Articles 4 (Pandemic prevention and public health surveillance) and 5 (Strengthening pandemic prevention and preparedness through a One Health approach)
Member State Consultation on the Investment Round
INB Informal meeting on Article 12 (Access and Benefit sharing)
INB Informal meeting on Article 11 (Co-development and transfer of technology and know-how)
WHO 18 September
INB Informal meeting Article 11 (Co-development and transfer of technology and know-how)
INB Informal meeting on Articles 4 (Pandemic prevention and public health surveillance) and 5 (Strengthening pandemic prevention and preparedness through a One Health approach)
WHO 19 September
INB - WGIHR Briefing on the financing landscape
WHO 21 September
Member State consultation on MS-led governance reform (follow-up to AMSTG)
WHO 22 September
Resumed meeting of the INB drafting group
V. NEWS FROM US:
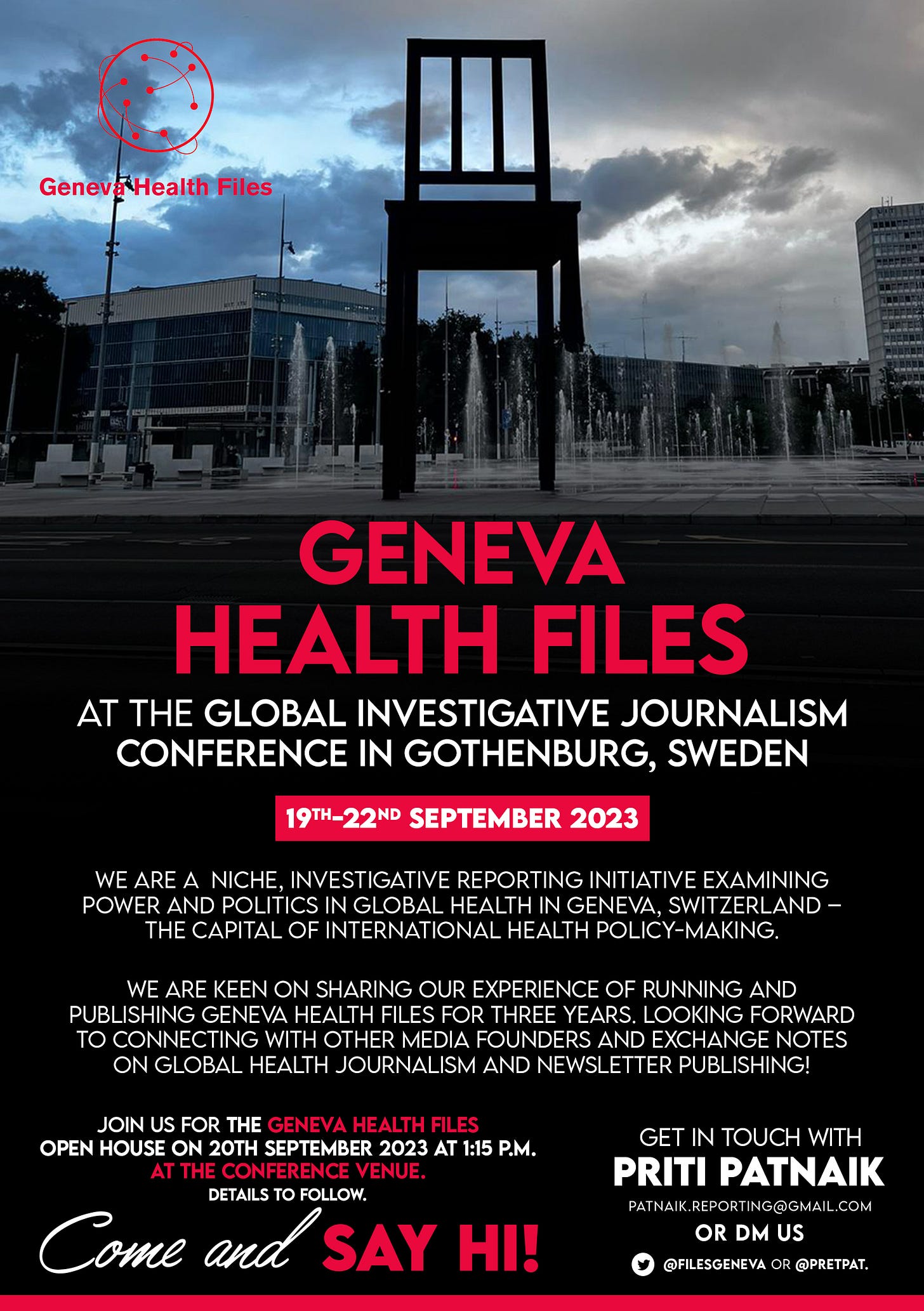
Geneva Health Files at the Global Investigative Journalism Conference:
Global health is everybody’s business. Help us probe the dynamics where science and politics interface with interests. Support investigative global health journalism.